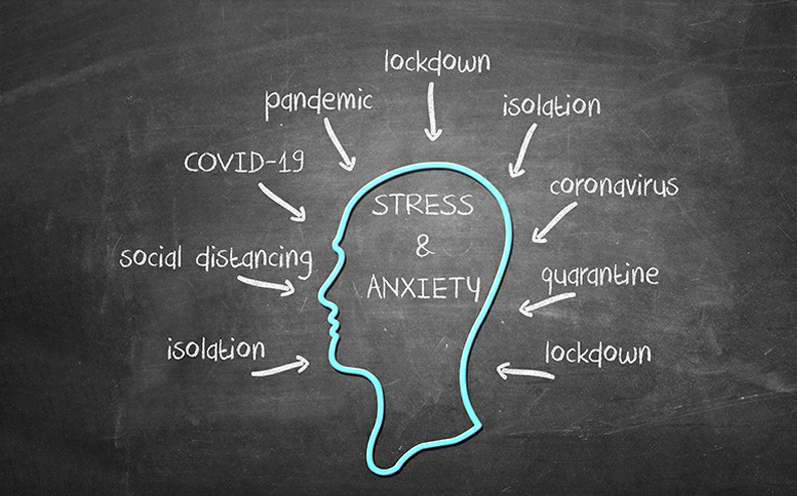
Struggling to return to a state of “normal?” You’re Not Alone.
The COVID-19 pandemic has dramatically altered our lives in nearly every way. In addition to many changes to our everyday lives – like social distancing, self-isolating, challenged work and school conditions, and strained social connections, to name a few – the pandemic introduced new levels of fear as well. Fear of getting sick (or worse), not just for ourselves but other loved ones. For some, worst fears became a reality as loved ones succumbed to their sickness.
With the pandemic slowly drawing to a close thanks to an increasing move toward herd immunity through vaccination, a renewed sense of normalcy appears on the horizon. But if you’re not quite feeling like your pre-pandemic self, you’re not alone. Mental health conditions have emerged for many. Could you be one of the many people struggling with a mental illness due to COVID-19? We explore the most common mental illnesses resulting from COVID-19 below.
Increased Anxiety
 A little worry from time to time is perfectly normal. But if you feel like you’re always worrying, even when everything is going fine, you may have an anxiety disorder. Current research estimates a three-fold increase in anxiety (at minimum) since the pandemic.
A little worry from time to time is perfectly normal. But if you feel like you’re always worrying, even when everything is going fine, you may have an anxiety disorder. Current research estimates a three-fold increase in anxiety (at minimum) since the pandemic.
“Having to deal with so much fear, stress and uncertainty can take a toll on our mental health,” shares Terri LaCroix-Kelty, MSW, Director of Munson Medical Center’s Behavioral Health Services. “The good news is that there are many ways we can focus on and improve our mental health so anxiety has less impact.”
There are several types of anxiety disorders. Common ones include:
- Generalized anxiety disorder (GAD). People with GAD worry too much. They also may have physical symptoms such as sweating or trouble sleeping.
- Panic disorder. Panic attacks are sudden bouts of extreme fear. Symptoms include rapid heartbeat, pain in the stomach or chest, difficulty breathing, excessive sweating, and more.
- Social anxiety disorder. People with social anxiety have a strong fear of embarrassment or judgment in social settings.
When anxiety won’t go away, it can begin to interfere with your daily life in a multitude of ways. Anxiety can impair your decision-making, affect your day-to-day activities, impact your work, and even keep you from connecting with friends and family.
Traumatic Stress Disorders
Post Traumatic Stress Disorder (PTSD)
 The COVID-19 pandemic was unquestionably a traumatic event for many people. Sometimes, the trauma we experience can continue to surface at unexpected moments even when we think we’re okay. With post traumatic stress disorder (PTSD), things that remind you of the traumatic event can make you feel as if you’re in danger again. These reminders are called triggers, which bring back memories, emotions, and physical reactions related to the trauma. Triggers can include not only sounds, smells, and sights but situations such as not hearing back right away from a loved one.
The COVID-19 pandemic was unquestionably a traumatic event for many people. Sometimes, the trauma we experience can continue to surface at unexpected moments even when we think we’re okay. With post traumatic stress disorder (PTSD), things that remind you of the traumatic event can make you feel as if you’re in danger again. These reminders are called triggers, which bring back memories, emotions, and physical reactions related to the trauma. Triggers can include not only sounds, smells, and sights but situations such as not hearing back right away from a loved one.
Symptoms of PTSD typically last more than a month. They may include:
- Unwanted or intense memories of a trauma
- Nightmares
- Vivid memories (flashbacks) that make you feel like you’re reliving the event
- Feeling worried, fearful, anxious, or suspicious
- Strong reactions when you’re reminded of the trauma (or sometimes for no obvious reason at all)
- Intrusive thoughts about combat, death, or killing
- Feeling disconnected or isolated, as if you’re “not yourself”
- Loss of interest in things you once enjoyed
- Feeling agitated, tense, on edge, or easily startled
- Bursts of anger or irritation
- Problems concentrating
- Trouble falling or staying asleep
Secondary Traumatic Stress Disorder
 You don’t always have to experience distress firsthand to feel its emotional impact. Secondary Traumatic Stress Disorder – also commonly referred to as “compassion fatigue” – can occur by the simple act of hearing another person’s traumatic account. Accordingly, you may even find yourself reliving the person’s shared experience. With an ongoing flurry of distressing COVID-19 headlines coupled with stories of loss, secondary traumatic stress disorder is another looming consequence of the pandemic. The symptoms closely mimic those of PTSD and can also include guilt, hypervigilance, and even physical ailments.
You don’t always have to experience distress firsthand to feel its emotional impact. Secondary Traumatic Stress Disorder – also commonly referred to as “compassion fatigue” – can occur by the simple act of hearing another person’s traumatic account. Accordingly, you may even find yourself reliving the person’s shared experience. With an ongoing flurry of distressing COVID-19 headlines coupled with stories of loss, secondary traumatic stress disorder is another looming consequence of the pandemic. The symptoms closely mimic those of PTSD and can also include guilt, hypervigilance, and even physical ailments.
Special types of therapy such as cognitive behavioral therapy (which focuses on changing negative thinking patterns) or eye movement desensitization reprocessing therapy (EMDR) can help you safely navigate these stressors.
“These therapies have been known to change brain functioning by rewiring neuronal tracks according to the latest neuroimaging research,” explains Dr. Michael Lucido, PhD, a clinical psychologist with Munson Healthcare Charlevoix Hospital. “It may be helpful to call ahead to determine if there is a therapist who would be able to treat this specific condition.”
Depression
Feeling sad occasionally is a part of life. But for people with depression, these dismal feelings interfere with daily living. Work, friendships, and self-care may suffer. Sadness is one symptom of depression, but there are many others. Have you experienced any of these signs for at least two weeks?
 You don’t enjoy the things and activities that you used to like, or they’re not as fun as they used to be
You don’t enjoy the things and activities that you used to like, or they’re not as fun as they used to be- You feel empty, worthless, or helpless
- You have trouble concentrating or making decisions
- You’re fatigued, even after sleeping well
- You’re thinking of hurting yourself
Depression is a whole-body illness. It involves the body, mood, and thoughts. Depression affects the way you eat and sleep. It also can affect the way you feel about yourself and things. It's not the same as being unhappy or in a “blue” mood. It is not a sign of personal weakness or a condition that can be willed or wished away. When you have depression, you can’t “pull yourself together” and get better. Treatment is often needed and many times crucial to recovery.
Addiction
Sometimes when we experience something traumatic, we turn to substances as a way of coping. If you find yourself drinking more alcohol or turning to drugs like opioids, marijuana, or other controlled substances as a result of the pandemic, you may be struggling with addiction. Addiction can also happen in response to other pleasurable things that stimulate the brain’s reward center, such as eating, sex, gambling, smoking, and surfing the internet.
Addictions can feel soothing because they help mimic the brain's own natural feel-good chemicals. Over time, our brains are rewired into believing that the addiction is a good thing and that we need it to survive. This rewiring is very strong. In fact, over time, you may discover that you no longer find pleasure in other things you once enjoyed because the addiction is more powerful.
Grief and Loss
Grief is what you feel when you lose someone or something dear to you. In the aftermath of the pandemic, you may be grieving anything from the loss of a loved one to the loss of experiences – or even what your children or grandchildren missed out on this past year. How long you grieve is a personal journey that has no right or wrong time limits.
When you grieve, it’s normal to have intense and enduring feelings of disbelief, shock, despair, sadness, and guilt that can be hard to cope with. While these feelings are a normal part of the healing process – and we need to process them to heal – they can be very unsettling.
Treatment and Support Can Help You Get Your Life Back
 If you’re struggling with any of these mental health conditions, or you just don’t quite feel like yourself and you’re not sure what’s wrong, please make an appointment to see your healthcare provider. He or she can make sure there’s no physical problem causing your symptoms and help you find an effective treatment, such as counseling, appropriate medication, and alternative treatment methods. You can also reach out to a trusted loved one – or even contact a help line for support.
If you’re struggling with any of these mental health conditions, or you just don’t quite feel like yourself and you’re not sure what’s wrong, please make an appointment to see your healthcare provider. He or she can make sure there’s no physical problem causing your symptoms and help you find an effective treatment, such as counseling, appropriate medication, and alternative treatment methods. You can also reach out to a trusted loved one – or even contact a help line for support.
You may think that asking for help is a sign of weakness. In fact, taking action to make your life better takes a lot of courage. Talking about a trauma can be hard, but it can make a significant difference in how you feel moving forward.
Your Mental Health Matters
Ready to get started on your journey to a better-feeling you? Find local, confidential, and in some cases, FREE resources for mental health, substance use disorder, and more.


In Distress and Need Immediate Help?
The National Suicide Prevention Lifeline provides free, confidential, 24/7 emotional support to people in suicidal crisis or emotional distress.Call or text 988 and speak to a counselor today.
Related Blogs: