
It started as a normal spring day for Sue Sawusch of Traverse City.
Sue and her husband Dirk saw declining COVID-19 numbers back in March 2021 as a chance to grab a bite to eat downtown. Nothing unusual for the couple. At least not until they returned home to relax.
After sitting down on her living room recliner, Sue realized she couldn’t get up.
“I thought it was my back,” the 61-year-old remembers. But Dirk knew right away. Something was wrong.
Sue was having a stroke. And suddenly, every minute mattered.
Signs of stroke? Call 9-1-1
Dirk noticed Sue was showing weakness in her left arm. She also was unable to support herself on her left leg. Recognizing signs of stroke, Dirk immediately called 9-1-1.

 An ambulance arrived and EMTs began an assessment while rushing Sue to Munson Medical Center. She remembers arguing with an EMT about whether she was having a stroke. Even then she didn’t believe it. Since there was no family history, a stroke didn’t seem possible.
An ambulance arrived and EMTs began an assessment while rushing Sue to Munson Medical Center. She remembers arguing with an EMT about whether she was having a stroke. Even then she didn’t believe it. Since there was no family history, a stroke didn’t seem possible.
Arriving at the medical center, a trauma nurse asked Sue if she could lift her left arm. “Of course,” she replied. But she couldn’t, even though she felt like she was.
Multiple CT scans confirmed Sue was suffering from two separate blood clots - one blocking her right internal carotid artery and a second blocking her middle cerebral artery.
In clinical terms, she was suffering from a tandem occlusion to R ICA and MCA. This is the most severe type of stroke one can have. Left untreated, a tandem occlusion can lead to brain swelling, severe disability, and death.
Successful clot removal
Ischemic strokes – those caused by blockages in blood flow to the brain – require fast treatment. Millions of Sue’s brain cells were dying every minute her brain lacked oxygen.
The medical center stroke team administered a clot-dissolving drug called Alteplase (or tissue plasminogen activator, known as tPA), but the plaque and clots were too large for the drug to have the desired effect.
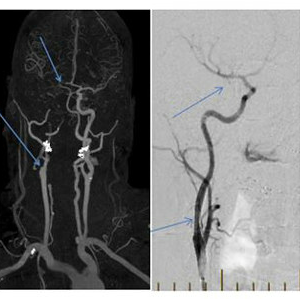
To make matters worse, tandem occlusions are difficult strokes to treat. Once the clots are removed, a stent must be placed in the carotid artery to encourage blood flow through the hard plaque to the head.
The only option was opening the carotid artery in Sue’s neck and blocked brain artery via intracranial thrombectomy — a minimally invasive procedure allowing a trained neurosurgeon to use microscopic instruments to remove the blockages and restore blood flow. The procedure is performed with only mild sedation in most cases.
Image right: (Left) Blocked blood vessels. (Right) Normal blood flow is restored after intracranial thrombectomy (clot removal) and carotid artery stenting.
Performing a thrombectomy
 Gary Rajah, MD, Cerebrovascular/Endovascular Neurosurgeon and Director of Munson Healthcare’s Endovascular Stroke Program, was called in to perform Sue’s thrombectomy. He carefully threaded a small retriever through Sue’s groin artery and into the blood vessels to her brain. Real-time imaging from Munson Healthcare’s Artis Icono Biplane machine allowed Dr. Rajah to eliminate both blockages – with full crisp visibility of the hair-like surgical instruments within Sue’s paper-thin intracranial blood vessels.
Gary Rajah, MD, Cerebrovascular/Endovascular Neurosurgeon and Director of Munson Healthcare’s Endovascular Stroke Program, was called in to perform Sue’s thrombectomy. He carefully threaded a small retriever through Sue’s groin artery and into the blood vessels to her brain. Real-time imaging from Munson Healthcare’s Artis Icono Biplane machine allowed Dr. Rajah to eliminate both blockages – with full crisp visibility of the hair-like surgical instruments within Sue’s paper-thin intracranial blood vessels.
“Stroke thrombectomy offers patients and families a chance of hope in their darkest hours,” Dr. Rajah said. “A timely thrombectomy can be the difference between severe physical and mental impairment with 24/7 assisted care for decades versus returning to work, life, and family in a functional and independent state.”
Although she can’t recall much, Sue remembers recovering in the ICU feeling relatively well. The procedure was a success.
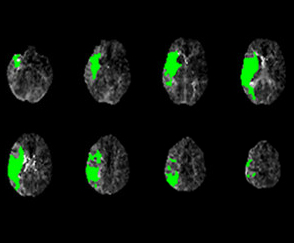
Image right: Sue’s severe stroke appears in green, encompassing nearly the entire right side of the brain.
Stroke post-op recovery and back to “normal”
 “Dr. Rajah was amazing,” Sue said. “Every morning he would visit my recovery room to reassure me and make sure I knew things were going to be ok. His entire neurovascular team was very kind.”
“Dr. Rajah was amazing,” Sue said. “Every morning he would visit my recovery room to reassure me and make sure I knew things were going to be ok. His entire neurovascular team was very kind.”
Dr. Rajah also let Sue’s husband Dirk into the angiography suite after the procedure to show him scans and explain what she had been through. This helped Dirk understand what led to Sue’s thrombectomy and helped to alleviate some his natural fear and anxiety.
“I didn’t know if I was imagining it or not, but I had this vision of Dr. Rajah explaining that the procedure was like Pac-Man eating up the blood clots. When I asked him about it, he smiled… But he didn’t respond either way,” Sue laughed.
After five days in the hospital, Sue walked out on her own. She completed six weeks of physical therapy to work on left leg and balance issues at a nearby Mary Free Bed at Munson Healthcare facility in Traverse City.
Sue's Life Today
Today, Sue is back to doing almost everything she used to do, although a little bit slower than before. She still has some weakness in her leg and she continues working through tremors and neuropathy in her feet. However, she uses no assistive devices and is fully independent.
“I’m really glad Dr. Rajah’s here,” Sue added. “Otherwise, I would have been transferred to another hospital and risked significant brain damage.”
What’s next for Munson Healthcare’s endovascular stroke program
 “A year ago, no stroke thrombectomy had ever been done in Northern Michigan,” Dr. Rajah said. “These cases would require a helicopter transfer downstate, putting brain cells and patient outcomes at risk. Today I’m happy to share we have done more nearly 200 right here in Traverse City for northern Michigan visitors and residents.”
“A year ago, no stroke thrombectomy had ever been done in Northern Michigan,” Dr. Rajah said. “These cases would require a helicopter transfer downstate, putting brain cells and patient outcomes at risk. Today I’m happy to share we have done more nearly 200 right here in Traverse City for northern Michigan visitors and residents.”
“We’ve linked all eight Munson Healthcare hospitals into one large regional stroke network covering the northern half of Michigan. We’ve also successfully performed hundreds of additional neurovascular procedures since the program started, including treatments of ruptured aneurysms and blood vessel malformations in the brain and spine.”
A variety of next steps are planned to help the stroke program expand. This includes continuing community education and recruiting more specialists to help with stoke diagnosis, treatment, and rehabilitation. Outpatient stroke services will also be added to help patients recover quicker and better.
The program also added another endovascular care suite featuring a second Artis Icono Biplane. That makes Munson Medical Center the only hospital in the country with two Artis Icono Biplane imaging labs.
Ultrasound Technology to Detect Blood Clots
 The hospital also acquired an ultrasound technology that allows physicians to evaluate the circulation of blood around the brain. This testing helps detect strokes caused by blood clots and reveals blood vessel narrowing, tiny blood clots, and more.
The hospital also acquired an ultrasound technology that allows physicians to evaluate the circulation of blood around the brain. This testing helps detect strokes caused by blood clots and reveals blood vessel narrowing, tiny blood clots, and more.
Munson Medical Center’s dedicated stroke unit and specialized nursing staff continues to care for stroke patients and promote their best possible outcomes.
“Hard work, teamwork, community help, and perseverance have led to the amazing first year success of this stroke program,” Rajah said. “I would like to thank all contributing staff and community members who made this much needed program succeed even during a global pandemic.”
“This program has and will continue to be transformative for community health in Northern Michigan.”